Growing pains: the need for realignment in the way we diagnose and treat musculoskeletal pain

A growing demand for services related to the diagnosis and treatment of musculoskeletal (MSK) conditions is placing increasing and significant pressures on the healthcare system. Tom Fleet, Senior Consultant, Strategic Advisory at Archus and a Physiotherapist with a background in specialist MSK triage and management discusses how we can realign the way we plan and design healthcare services for MSK patients.
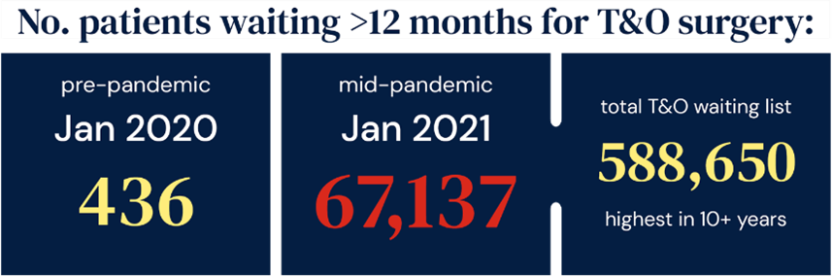
In both primary and secondary care, musculoskeletal (MSK) conditions account for a significant amount of demand. There are several prevalent health risk factors driving the demand for MSK care, but the system is also seeing the impact of an aging population, who depend on maintaining functional ability as part of the healthy ageing process[⁶]. The Covid-19 pandemic further exacerbated the impact of MSK demand, with a significant backlog of over half a million patients now awaiting Trauma and Orthopaedic (T&O) input, the highest in more than ten years.

Diagnostic Imaging (DI) techniques, such as Magnetic Resonance Imaging (MRI) or X-Ray, have historically been used to find the “root cause” of those presenting with MSK symptoms. For example, if an individual has a painful shoulder, then the clinician may scan the shoulder to diagnose and guide treatment for the problem. Interestingly, in the context of a growing number of patients experiencing symptoms of MSK conditions, demand for DI has increased disproportionately, with a 16% growth in referral rate for DI across the NHS between 2014 and 2019[¹⁰]. In an increasingly capital-constrained environment, this presents major implications. In response to the growing demand for DI, the 2021 Autumn Spending Review announced £2.3 billion in investment over three years to transform diagnostic services, with at least 100 community diagnostic centres across England, as part of an effort to tackle the diagnostics backlog.
A knotty issue
One might assume that a growth in the rate for Diagnostic Imaging (DI) is logical in the context of a growing rate of MSK conditions. However, several industry leaders have identified that the rate of growth is, in fact, not justified by Clinical Practice Guidelines from across the UK. It is suggested that clinician behaviour and patient expectations are the drivers for the increase, rather than robust clinical rationale[³]. Guidance administered by The Royal College of Radiologists have provided clear guidance[¹⁵] on MSK imaging referrals, in part to mitigate the growing demand for imaging services by setting out limited and explicit reasons to justify referral for DI for MSK conditions.
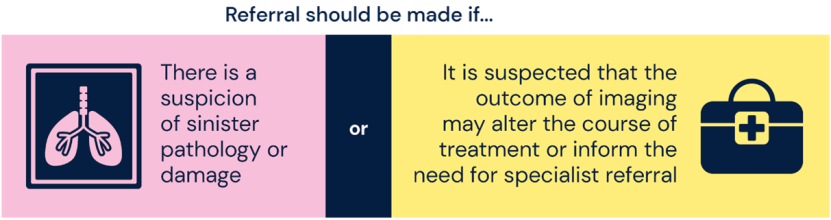
The rationale behind this clear guidance is simple. In many cases diagnostic images taken of painful joints or tissues do not correlate with clinical symptoms or functional impairment, offering little to no value to the patient or their recovery[³]. In addition, for many MSK ailments, such as low back pain, robust evidence demonstrates that regardless of the results of DI, guidance on the management of the condition is unchanged[²,⁴]. Research suggests similar findings for shoulder and knee pain[¹,⁷].
In some cases, DI may even hinder recovery, reinforcing an approach which portrays MSK pain as a direct effect of physical damage. For example, evidence shows that those who undergo MRI for low back pain are at risk of experiencing worse clinical outcomes compared to those who do not have imaging, and patients who have imaging are more likely to go on to have surgery[⁴,⁸]. Through imaging MSK conditions inappropriately, a clinician risks hindering a patient’s self-driven approach to resolving their issue through an empowering, tailored plan that has self-management at the core[¹⁴]. This is inconsistent with the integrated and holistic models of delivery and the overall ‘left shift’ of healthcare which is envisaged within the Long-Term Plan.
All of this raises important questions around the justification of expensive and higher-risk procedures when the rationale is largely influenced by subjective factors and the results so often refute any mechanical explanation for symptoms. A sustainable model of delivery to address this must be found.
A key challenge for clinicians in considering this evidence is that an individual’s experience of MSK pain is subjective, making solutions more difficult to determine. In many cases, pain cannot be reduced to a single cause, creating a unique experience for each person where the relationship between pain and damage is complex, and far from linear. DI is unlikely to be the answer.
Examples of this abstract nature of pain are commonly seen in everyday clinical practice. For example, an osteoarthritic knee may function well and give little discomfort to the individual, whereas a normal-looking knee on X-Ray could produce severe symptoms[⁵]. The patient with osteoarthritis may be able to functionally continue without issue, and not require intervention. Conversely, the patient with a normal X-Ray may be perceived to require more invasive intervention, such as an injection or surgery. This is driven by experiencing higher levels of pain rather than proportional damage.
So why is there a greater propensity to refer patients for DI? Conversations between patient and clinician to promote alternative routes of management can be confronting for both parties but are vital to reach a shared understanding. A refusal to refer patients for DI who have been suffering with persistent, severe pain can be challenging, particularly when that individual is desperately seeking a solution. The infrastructure must also be in place to empower and support clinicians in providing an alternative pathway for patients, whilst enhancing the visibility of the principles of good practice.
Realignment: a patient-centred and integrated solution
As healthcare professionals we are increasingly understanding of the fact that pain is not always the direct result of a physical issue but can be influenced by a range of psychological, social, or lifestyle factors[⁶,⁹].
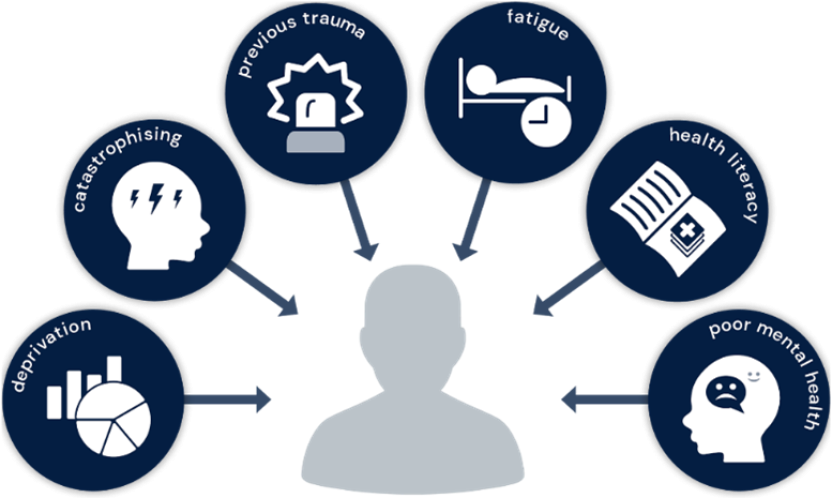
This means that exploring the wider psychological, social, and lifestyle factors that matter to an individual can be equally effective for supporting long-term recovery. This holistic, multi-faceted approach requires the clinician to draw on a wider network of health services which can help address the broad influencers of MSK pain, such as weight management, mental health support, and services which promote activity and wellbeing, to truly encompass what matters to a person’s recovery.
The benefits of this method of delivery are that it recognises the person, not just the pain, and encourages them to take responsibility while receiving support to improve their overall wellbeing. It supports both person-centred care and enhanced clinical outcomes, alongside the reduction of unnecessary cost associated with diagnostic procedures and secondary care services. This has far-reaching benefits to the individual and society, beyond improving MSK health alone.
Such an approach is supported by the NHS Long Term plan, which outlines a shift towards community-based, personalised care, where wider community services take a more prominent role in healthcare delivery. The formation of Integrated Care Systems (ICS), which aim to deliver care across a range of services, tailored to the local population, with improved accessibility and a reduced emphasis on the traditional hospital-centric model also aligns with this approach.
The ongoing maturation of ICS structures may go some way to facilitating this change. The ICS design framework sets clear expectations that the voluntary, community, and social sector should be involved in shaping, improving, and delivering services as an Integrated Care Board strategic partner, developing, and delivering plans to tackle the wider determinants of health. However, these changes will only be effective as ‘top-down’ strategy if they are put into practice in a ‘bottom-up’ method of delivery. It is only through this combined change that a fundamental alteration can take place.
Healthcare planning and design: the backbone of transformation for MSK services
When considering the evidence-based theories outlined in the context of the current Orthopaedic and diagnostic caseload, one could speculate that there are many patients currently within these services who could otherwise be managed alternatively. However, this issue is not for MSK teams and clinicians to resolve alone. Healthcare Planners and clinical leaders involved in the planning and development of services and infrastructure have a key role to play.
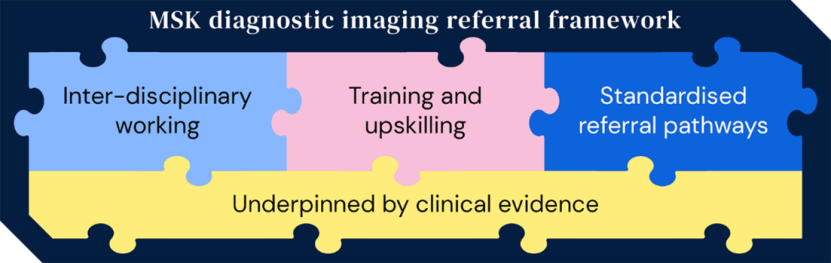
By taking a critical view of existing MSK systems and referral pathways for DI and then redeveloping these approaches using current, evidence-based guidance as a foundation, we can be an enabler in unlocking a more progressive approach to MSK management which places far less emphasis on DI.
How might this look in practice?
Clinicians with imaging referral rights should receive substantial training upon moving into these roles to ensure consistency in approach, with systems should be in place to facilitate the auditing of clinician’s imaging referral rates. The nationally mandated creation of a safeguarded set of skills for First Contact Practitioners and MSK Triage teams has been a step towards achieving this. A safeguarded level of skill should be hard-baked into proposed new pathways or systems of care delivery.
Secondly, an iterative relationship between the diagnostic radiology and MSK team will also help promote the appropriate use of imaging and reject inappropriate use. This should involve the promotion of standardised referral pathways with explicit criteria, a change already advocated in NHS improvement guidelines[10]. As well as this, establishing inter-disciplinary shared learning forums, also cited in this guidance, gives the opportunity for clinicians to build confidence, skills, and knowledge to uphold a high standard of practice. Digital technology can play a key role in facilitating this collaborative approach. Archus has extensive experience in delivering bespoke solutions to realise connectivity and visibility between different components of the care pathway.
Next, those delivering transformation to MSK services must consider the wider system within which the service sits. By providing a robust network of support services to cater for a holistic approach, a clinician can feel empowered to promote a non-medicalised and wholistic pathway for a patient experiencing MSK pain. Without these services at their disposal, a clinician may be driven by a desire to provide the patient with some form of appeasement by referring them for DI, even in the knowledge that it may be unhelpful. As Healthcare Planners, we must explore if, and how accessibly, these services interface with the MSK service, understanding the barriers to both awareness and utilisation by MSK clinicians.
An example of an organisation harnessing this improved linkage with the wider system is Live Life Better Derbyshire, an initiative funded by Derbyshire County Council.
This service can be accessed directly by patients or referred into by clinicians. Organisations such as this are invaluable as a resource for clinicians working with patients with MSK and other multi-faceted health complaints, as all the services offered can impact not only MSK pain, but overall wellbeing. Though the initial cost of broadening the local offering of services such as this may be high, the resultant longer-term reduction in the demand for orthopaedic and other consultant-led NHS services could be incomparable.
Perhaps most importantly, we need a significant realignment in thinking regarding the health building environment for MSK services. Modern principles of healthcare design, spurred by the NHS Long Term Plan, dictate a need for services to be housed at locations offering greater integration with local communities.
Since 2021, Archus have supported several “pioneer” sites in the Cavell Centre programme, providing services for healthcare planning and business case authorship. These community hubs will offer a range of co-located and fully integrated health and social care services such as community services, outpatients, and other NHS services in addition to third sector and Local Authority services. They aim to help people live longer with healthier lives, supporting self-care, and empowering people to manage their own health conditions better, reducing inequalities.
Not only does this approach provide improved accessibility for many, but it can also be a vital component in reinforcing the idea that not all MSK pain needs to be “treated” in the traditional, medical sense which is commonly associated with attending a hospital or acute environment. In addition, such facilities better recognise the complex relationship between pain, damage, and psychological, lifestyle, or social factors and are likely to be better suited to the successful management of MSK pain, reducing the overall demand on secondary health services and improving patient outcomes. They also present the opportunity to harness a diversified workforce, recognising that a broad scope of staff, such as those qualified in Sports Rehabilitation or Personal Training, may be in a strong position to support the delivery of MSK care.
Whether considering physical health building design or less tangible models of care, we should continually be challenging ourselves to consider what messages we are giving to a patient when they attend their MSK appointment, particularly in relation to DI. Pathways should be designed to protect this high-tariff, high-demand resource. By promoting standardised, trusted, and agreed pathways in the planned and unplanned setting, which give clear decision-making support to clinicians, we can collectively drive the message of appropriate use of diagnostic resources.
The Archus team has a vision for achieving market-leading, patient-centred healthcare at its core. Clinicians and transformation leaders within the business are experienced at offering their expertise to give tailored support to organisations seeking an evolution of their current clinical pathway delivery. By using evidence to underpin and integrate the development of modern models of care, transformation to the practices followed by clinicians, and the supporting infrastructure of the healthcare estate, healthcare planners can reduce the demand that MSK conditions are placing on the health system, safeguard an overall improvement to MSK care, and create better clinical outcomes for patients.
Our expert team work with healthcare systems and providers to implement affordable and achievable strategies which improve service delivery and health outcomes for both the short and long-term, realising tangible change.
To start a conversation about how we can help you, get in touch.
Further reading and references
